A viscosupplement administered as an injection by a clinician. To determine if the dietary supplements, glucosamine and/or chondroitin, result in reduced joint space narrowing (jsn) and pain among people with symptomatic knee osteoarthritis.

Acute Emergencies Related to Systemic Disease and How They
Ideally a person should avoid arthroscopy.

Medial joint space narrowing knee treatment. Viscosupplementation is a treatment option for joint space narrowing secondary to osteoarthritis. Jsn can cause pain, and pain relief medication is. Large variability in medial compartment joint space narrowing (jsn), in relation to the mean jsn, in previous studies of
Bmi was found to have a distinct effect on the association of mjsw with pain. Radiography is a commonly accessible tool for assessing knee osteoarthritis, especially in. The gel used for injection can be either from animal or made synthetically.
Knee joint space narrowing treatment ross hauser, md surgery damages cartilage leading to further pain, injury and quickens the arthritis process. Prevention of medial compartment osteoarthritis lose just 10 pounds and you’ll take as much as 40 pounds of force off your knees. A doctor can use this to assess the severity of the arthritis.
But if arthroscopic surgery has already happened, prolotherapy is a good option to halt the arthritic process.oral antibiotics are usually used in the treatment of gonococcal. This substance helps to lubricate the knee joint and can decrease the amount of inflammation. Avoid activities that aggravate symptoms as much as possible whilst still getting on with daily life.
I would recommend you talk to your doctor for. This is replacement of only the medial side of your knee. Cultures of the joint fluid used to id the specific bacteria, which guides antibi.
He did order an mri. An orthopaedic surgeon will remove a portion of either the shin bone or the thigh bone to offset the distribution of weight on the knee joint, which can help relieve pressure on the side of the joint that has begun to suffer damage. The threshold of medial mjsw was approximately 3 mm in men and 2 mm in women, while that of medial mjsw/lateral mjsw was approximately 60% in both men and women.
A bedside arthrocentesis was performed in the emergency department and sent for fluid analysis with complete results listed in table 1. Arthroscopy of the osteoarthritic knee is a common and costly practice with limited and specific indications. Joint space narrowing can also be a result of conditions such as osteoarthritis (oa) or rheumatoid arthritis (ra).
Gel injections are another treatment option in cases of joint space narrowing. Acetaminophen (tylenol) for pain relief, if nsaids are not suitable. Described in animal models of knee osteoarthritis and in humans [1].
The main compound of the gel used for such a treatment is hyaluronic acid. But, there are steps you can take to slow the progression of underlying osteoarthritis and reduce painful symptoms. I go into a lot more detail about htos in this post.
If you feel abnormal pain in your. Cartilage is taken from a different area in the knee or body and used to fill the space. In addition, joint space narrowing was evaluated not by categorical grade but by continuous values, using mjsw at the knee.
Often, films will be taken with the patient supine, which gives a false sense of joint space and alignment and should not be used to evaluate suspected knee oa. This gives an accurate representation of the joint space narrowing present. The extent of osteoarthritis (oa) is determined by joint space narrowing.
Both half and total knee replacements are available. There is no cure for subchondral sclerosis. No injuries to my knowledge except for doing a lot of high intensity cardio for a year and half, which thinking about it now, is pretty rough on knees.
In serial radiographs of the knee with oa, hypertrophic repair may present as widening of the joint space (wjs). Obviously you are very young to have arthritis, unless you've had prior significant trauma to your knee. , though the threshold of joint space width for pain remained unclear.
Sex and bmi affected the association of medial mjsw with knee pain. In most cases, surgery is not required. My ortho didn’t really say a whole lot about it.
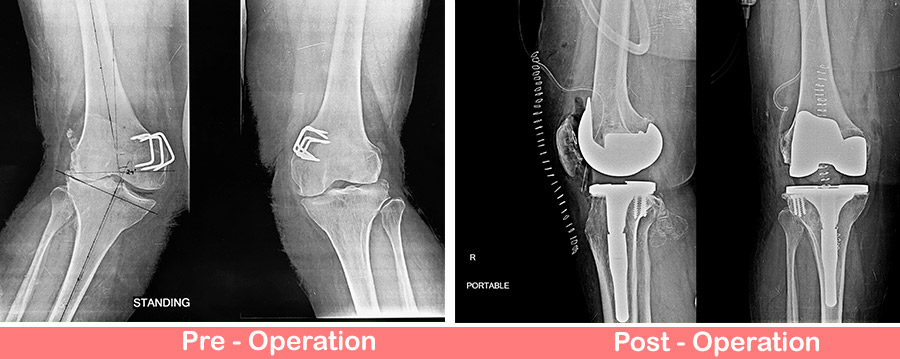
Treatment for patellofemoral arthritis usually starts with conservative methos i.e. One of the most gratifying surgical treatments for medial joint space narrowing is called a high tibial osteotomy, or hto. Total knee replacement (tkr) surgery is commonly used to treat those patients with intractable symptoms of knee osteoarthritis after conservative treatment failure.
Extreme cases may benefit from knee replacement surgery. People with knee osteoarthritis can experience close to double the amount of degradation compared to the level of cartilage loss in a healthy knee over the same period of time. A condition such as arthritis will cause the space to narrow.
It is important to understand that radiographs of the knee must be obtained with the patient standing. The osseous structures were intact without fracture, dislocation, or bony erosions.
Generally, treatment for an avulsion fracture includes: Management and treatment how are avulsion fractures treated?
Medial collateral ligament avulsion femur Image
Posterior cruciate ligament avulsion fracture;
Avulsion fracture knee treatment. In this avulsion fracture treatment, a cast is placed on the fractured area for anywhere from four to six weeks. The knee joint remains particularly susceptible to avulsion fractures due to its numerous tendinous, ligamentous, and meniscal attachments. Anterior cruciate ligament avulsion fracture;
Injuries like this, if gone untreated, can lead to further damage and lifelong pain. However, conservative treatment often causes some complications, such as synarthrophysis, nonunion, joint instability, and arthritis, resulting in an unstable fixation and an unsatisfactory outcome. Treatment of an avulsion fracture typically includes resting and icing the affected area, followed by controlled exercises that help restore range of motion, improve muscle strength and promote bone healing.
How is avulsion fracture of the knee treated? How long does it take to recover from an. Arthroscopically loop or transosseous can be fixed.
However, if the fracture is. Clinical and radiographic findings confirmed the presence of an avulsion fracture at the proximal attachment of the mcl, combined with complete anterior cruciate ligament (acl) and posterior cruciate ligament (pcl) rupture. The treatment method was not standardized and was determined by the patient, their parents, and the treating physician regardless of the presence of avulsion fracture.
Origin of mcl avulsion fracture: Most avulsion fractures respond very well to physiotherapy treatment & only severe cases require surgical intervention. But in the condition of, even though very uncommon, tibial tubercle avulsion fracture, surgery gives a better outcome and resolution.
Doctors also recommend that this be paired with ice therapy, where ice is applied to the injured area for 20 to 30 minutes every three to four hours, or during times of swelling or pain. Most avulsion fractures are treated conservatively with pain and swelling control and early return to activities. Keep weight off the ankle until it has healed, and take measures.
Most avulsion fractures heal very well without surgical intervention. Treatment depends on which bone broke and the type of avulsion fracture. Displaced avulsion fractures require surgery.
Avulsion of the medial collateral ligament. To find out more, contact naas physio clinic on: Commonly, conservative treatment and surgery are the two major treatments of avulsion fracture.
An avulsion fracture occurs when a small chunk of bone attached to a. If the fracture is small, it can be treated with as little as rest, ice, and a bandage. Removing small portions of the kneecap that cannot be reconstructed may also have good results.
Avulsion fractures of the knee are numerous due to the many ligaments and tendons inserting around this joint. If the kneecap is broken in many pieces at its center and the pieces are separated, your doctor may use a combination of wires and screws to fix it. Immobilization in a cast or splint.
An avulsion fracture involves the detachment of a bone fragment that results from the pulling away of a ligament, tendon, or joint capsule from its point of attachment on a bone. Complete removal of the kneecap is a last resort in treating a comminuted fracture. Open reduction and internal fixation with a screw can be done.
The main treatments for an ankle avulsion fracture are rest and icing. Ofter bracing or splinting are used. Treatment of an avulsion fracture typically includes resting and icing the affected area, followed by controlled exercises that help restore range of motion, improve muscle strength and promote bone healing.
Even a small bone chip (avulsion fracture) should not be taken lightly. Most avulsion fractures heal very well without surgical intervention.
Also, the generated mixed fibrous cartilage tissue is not the same as. Osteoarthritis of the knee (koa) occurs when the cartilage — the joint’s natural cushioning system.
Plan Your Stem Cell Therapy for Osteoarthritis in India
By gabriella rogers • health reporter.

Stem cell treatment for osteoarthritis of the knee. Hundreds of australians are being recruited in a. Stem cell based therapy is an emerging field in orthopaedics. Traditional oa treatment (e.g., arthroscopic debridement, microfracture, autologous or allogeneic cartilage transplantation, chondrocyte transplantation) is primarily symptomatic treatment and pain management, which cannot contribute to regenerating degenerated cartilage or reducing joint inflammation.
Firstly, at approximately $4000 per knee for stem cell reinjection, which will not be covered by health insurance, this treatment is not for affordable by everyone. The objective of this study is to evaluate the effectiveness, safety and potential of mesenchymal stem cells (mscs) for knee osteoarthritis treatment. Mesenchymal stem cells (mscs) are known to have a potential for articular cartilage regeneration.
Ticles with the keywords of “treatment, stem cell, knee osteoarthritis” in the english language. (1) animal studies have reported that the expanded culture of mesenchymal stem cells (mscs) is conducive to repairing cartilage and subchondral bone, and regulating the progression of secondary osteoarthritis (oa); Mesenchymal stem cells for treating knee osteoarthritis.
Total knee replacement is commonly seen as the solution for severe knee osteoarthritis, but in recent years, stem cell therapy has emerged as a genuine alternative, offering a raft of advantages. To assess the clinical efficacy and safety of mesenchymal stem cell (msc) treatment for osteoarthritis of the knee (koa), a systematic electronic literature search was performed on pubmed, embase and web of science. A recent pilot study investigates stem cells as a potential treatment for osteoarthritis.
Regenerative medicine utilizing stem cells, platelet rich plasma (prp), amniotic fluid, and cytokine modulation is very promising in the treatment of koa. To review the current basic science and clinical literature on mesenchymal stem cell (msc) therapy for articular cartilage defects and osteoarthritis of the knee. Stem cells are produced by the body in the bone marrow, before being sent to where they are needed.
More challenges and barriers also exist when reviewing the trials involving knee osteoarthritis and stem cell therapies. However, there have been few midterm reports with clinical and structural outcomes. For the treatment of generalized cartilage loss in osteoarthritis, an alternative delivery strategy would be more appropriate.
Osteoarthritis (oa) is an inflammatory condition still lacking effective treatments. What is stem cell therapy for osteoarthritis? This study describes the treatment of knee osteoarthritis with cd34+ stem cells at the medical magnus outpatient clinic in lodz, poland, together with the treatment and rehabilitation algorithm developed for maximum effectiveness of this procedure.
However, most studies focused on focal cartilage defect through surgical implantation. Among the more innovative, experimental therapies, mesenchymal stromal cells (mscs) are proposed as a novel therapy with potential in treatment of koa. Stem cell therapy could also potentially treat osteoarthritis (oa) of the knee.
This can progress to osteoarthritis. Stem cells injection for knee osteoarthritis is still a relatively new treatment and has not yet gained popularity. Cartilage in the knee does not heal very well nor very quickly, so continued use of the leg when walking for example can result in further damage, bony projections (osteophytes), stiffening and swelling of the joint (fig.
(2) recent studies on the treatment of oa by mscs have progressed to clinical trials, and most clinical trials have. Secondly, there are several criteria for eligibility for treatment of osteoarthritis with stem cells preparations. This is a review article to evaluate the current evidence about regenerative medicine therapies in the treatment of koa.
Many trials combine therapies including platelet rich plasma, hyaluronic acid and others. In oa, the cartilage covering the ends of the bones starts to deteriorate and wear away. Stem cell injection for knee osteoarthritis (koa) is an emerging new therapy, and we aimed to review its evidence of efficacy.
Clean the skin on your knee and treat it with a local anesthetic insert the needle into your joint, which might cause some discomfort inject the medication into your joint Here’s the latest evidence on a growing range of options for treating oa pain, including topicals, pills, injectables, physical therapy, orthotic, brace care and more.
Hyaluronic Acid for Osteoarthritis Osteoarthritis
It was conducted a prospective study with a series of 153 patients treated with prp injections in patient affected by knee osteoarthritis.

Osteoarthritis knee injection treatment. Medical treatments for osteoarthritis pain. Ad veterinary medicine international invites papers on all areas of veterinary research. Physical modalities for the treatment of knee pain in patients with osteoarthritis include physical therapy, exercise, weight loss, and the use of braces or heel wedges.
Hindawi's academic journals cover a wide range of disciplines. According to the american college of rheumatology and arthritis foundation guidelines for managing knee osteoarthritis, corticosteroid injections are recommended over other types of injections due to better outcomes and effectiveness in alleviating symptoms. If you have tried all other nonsurgical treatment methods and your pain continues to limit your activities, viscosupplementation may be an option.
Knee osteoarthritis is a disease based on degenerative pathological changes [1, 2]. Scientists have found that a new knee injection using nanomedicine could prevent the effects of osteoarthritis. We are going to show the.
The arthritis foundation is proud to have partnered with the american college of rheumatology (acr) on the development and release of these guidelines for the management of osteoarthritis (oa) of the hand, knee and hip. Treatment is observation, nsaids, tramadol and corticosteroids for. Pain relief is usually obtained by.
One independent observer performed clinical and functional evaluations at t0 (recruitment), t1 (one month after the injection), t2 (three months after the last injection) and t3 (six months after the last injection). Primary care doctors, physical therapists and orthopaedists can play an important role in treating osteoarthritis. Another treatment option is a procedure called viscosupplementation.
2020 eular recommendations for the management of knee osteoarthritis support the use (recommended) of hyaluronic acid injections: Ad naturally heal knee osteoarthritis and relieve pain without surgery! Complementary and alternative medicine treatments that have shown promise for osteoarthritis include:
Consider hyaluronic acid injection for persistent knee osteoarthritis consider corticosteroid injection for acute exacerbation of knee osteoarthritis consider opioid therapy, but monitor carefully A group of scientists have discovered a potential method to cure osteoarthritis. Diagnosis can be made with plain radiographs of the knee.
By injecting this viscous fluid into an arthritic joint, viscosupplementation aims to reduce the friction and pain associated with moving an arthritic knee. Cortisone injections for knee osteoarthritis cortisone (also called corticosteroid , or steroid) injections are the most common type of injections. A doctor may suggest injections as a treatment for osteoarthritis (oa), which involves the erosion of joint cartilage and bone.
Some studies indicate that acupuncture can relieve pain and improve function in people who have knee osteoarthritis. The study was conducted at the university of pennsylvania, us. Bone marrow aspirate concentrate (bmac)treatment for knee osteoarthritis (bmac) the safety and scientific validity of this study is the responsibility of the study sponsor and investigators.
Unfortunately, the benefits of this treatment are still unclear. Knee osteoarthritis is degenerative disease of the knee joint that causes progressive loss of articular cartilage. They are the most commonly used knee injections for treating knee pain from osteoarthritis.
Listing a study does not mean it has been evaluated by. “there is evidence to support the efficacy of hyaluronic acid in the management of knee oa both for pain reduction and functional improvement” (pendleton et al., 2000). Whether it's corticosteroids or hyaluronic acid, injections may be a good treatment for your knee osteoarthritis.
According to the researchers, a simple knee injection could stop the disease’s effects.
In particular, patients with an early arthritis of the lateral femorotibial compartment or damage of the. Total knee arthroplasty (tka) is used to treat knee valgus deformity, and approximately 10% of all patients who require tka present with valgus deformity.

Valgus deformity of the knees. Download Scientific Diagram
Salter and best 91 reported that 10 of 13 patients with valgus deformity required tibial osteotomy for correction.
Valgus deformity knee treatment. Abdel, md, told attendees at icjr’s inaugural course for senior residents and fellows, advanced techniques in total hip & knee arthroplasty, whether they use cruciate retaining or posterior stabilized implants. Read more about treating rickets. Posted on november 3, 2015 september 15, 2016 by ryan nunley.
Mild knock knees that persist into adulthood don't need to be treated unless they're causing problems, such as knee pain. Aspirin hot bath with epsom salts menthol topical. In younger patients, an osteotomy surgical procedure may be an option.
These have been shown to kill off needed cartilage (1). Nineteen cases of osteoarthritis of the knee with valgus deformity in 17 patients were treated by femoral supracondylar varus osteotomy (17 cases) or by high tibial varus osteotomy (2 cases) over the last 15 years. A valgus painful knee is a disabling condition that can affect patients of all ages.
And after that, the opening which was made on the lateral side of the femur bone is done for the correction of valgum deformity and to bring back the knees into correct alignment. This involves cutting the femur, or thigh bone, to. Bone defects like lateral cartilage erosion, lateral condylar hypoplasia and metaphyseal femur and tibial plateau remodeling along with soft tissue pathologies like tight lateral.
Antivalgus osteotomy of the knee is the treatment of choice to correct the valgus, to eliminate pain in the young or middle age patient, and to avoid or delay a total knee replacement. Balthazar and pappas 5 pointed out that, even with osteotomies, the valgus deformity can recur. As far as problems go, it can lead to a lot of nasty injuries if left unchecked, and as a habit contributes to a less than desirable muay thai stance and legs that buckle under low kicks.
It occurs in young children (up to 7 years old), but during this period only observation and prevention are required since the musculoskeletal system is still being formed. At the age of 11 years, the diagnosis of valgus. Valgus knee deformity is a challenge in total knee arthroplasty (tka).
I illustrated with the example of valgus collapse of the knee, where the knee buckles inward under load… and this is pretty common in fighters. Side plank exercise side plank exercises strengthen the hip abductor muscles on the outside of the thigh. Nonoperative treatment orthotics/bracing is not effective in genu valgum.
Treatment overview pathologic genu valgum should generally be treated with surgery. If knock knees are caused by an underlying condition, treatment for this may be necessary. On the contrary, if your condition is severe, your doctor may recommend a more drastic treatment, i.e., knee replacement surgery.
Knee valgus also known as a knock knee or genu valgum. Patients within this physiologic range do not require treatment. This treatment is generally common in people aged 50 years and above.
A distal femoral lateral opening wedge procedure appears to be one of the choices for medium or large corrections and is particularly easy and precise if compared to the medial femoral closing. Such recurrence has been attributed to the same asymmetric overgrowth phenomenon that led to the valgus deformity initially. Surgery can correct the valgus deformity as well as the osteoarthritis that has accumulated in the knee joint over time.
A mild angle is <15°, a moderate degree is 15° to 30. That’s why it’s so important for surgeons to address varus or valgus deformity during the index surgery, matthew p. Strengthening the knee and hip muscles can improve a valgus knee.
For example, rickets can be treated with vitamin d and calcium supplements. As a result, someone with knee valgus will find it helpful to begin a program of frequently releasing and stretching these muscles. Most patients with valgus knee who end up with lateral compartment arthritis start with treatments like cortisone steroid shots.
The deformity can be caused by either bony or ligamentous pathology or both. As a rule, by the age of 7, the dynamics are already visible. Another less commonly explored treatment option for knee valgus is trigger point therapy.
1 a valgus deformity of the knee patient reports moderate pain (50%) 0 valgus deformity of the knee patients report mild pain (0%) 0 valgus deformity of the knee patients report no pain (0%) what people are taking for it. Valgus deformity in total knee replacement is a much lesser encountered problem than varus deformity. Treatment of severe genu valgus deformity.
Surgical intervention should be considered. Then metal plates are inserted where the cut has been made to stabilize the osteotomy or femur bone and further screws are used for tightness of that metal plates.