These mechanisms can cause this class of femur fracture. Surgeon uses the blunt site of the drill to pack the bone pulp tightly.

Lfc Knee / Plural, 3rd person singular present tense knees
Nondisplaced subchondral fracture is noted in the lateral facet of the patella.

Subchondral fracture lateral femoral condyle treatment. Alternate treatment approach to subchondral insufficiency fracture of the knee utilizing genicular nerve cooled radiofrequency ablation and adjunctive bisphosphonate supplementation: 15 we recommend deferring physical therapy immediately after diagnosis of a subchondral insufficiency fracture,. Subchondral fractures are usually a consequence of compressive forces, transmitted from the cartilage to the subchondral bone plate and from there to the trabeculae, which fail to resist that force and break or fracture 3.
No , what the doctor has recommended is weight bearing as tolerated, which is precisely what i have recommended.if something is causing pain, you may desist from doing it, but it will not affect your bone healing as well as the fracture, because the fracture is not in a weight bearing portion of your bone, so there is little you can do to stop it from healing.so, i. Percutaneous subchondroplasty of the medial femoral condyle insufficiency fracture; Excessive knee pivoting that causes a complete anterior cruciate ligament (acl) tear may result in a subchondral compression fracture on the lateral femoral condyle after impacting the lateral tibial condyle.
Typically, the knee and leg will be. While appropriate physical therapy regimens are important to improve on aerobic capacity, quadriceps muscle strength, or lower extremity performance, weight bearing may exacerbate subchondral fracture pain and could potentially prolong healing. Your programme will be tailored to your needs and goals and will involve a combination of approaches to optimise your recovery.
When a patient comes in with concern for a femoral condyle fracture, it is crucial to image the fracture first. The medical and lateral menisci are normal. Subchondral compression fracture on the lateral femoral condyle after impacting the lateral tibial condyle.
They can also occur in conjunction with twisting and ligamentous injuries. The patient was referred for a second course of bisphosphonate infusion treatment, and commenced this treatment at 12 months after her first presentation. Subchondral insufficiency fractures of the knee are commonly misdiagnosed fractures that are both very painful and difficult to treat.
The quadricepts tendon and patellar tendon are intact. Patients with osteoarthritis who want a nonarthroplasty While appropriate physical therapy regimens are important to improve on aerobic capacity, quadriceps muscle strength, or lower extremity performance, weight bearing may exacerbate subchondral fracture pain and could potentially prolong healing.15 we recommend deferring physical therapy immediately after diagnosis of a subchondral insufficiency fracture,.
Physiotherapy treatment following a fracture of the femoral condyle. Technique for treatment of subchondral compression fracture of the lateral femoral condyle associated with acl tear bone graft substitute for tunnel filling improved acl reconstruction outcomes clinical characteristics and outcomes after primary acl reconstruction and meniscus ramp repair Technique for treatment of subchondral compression fracture of the lateral femoral condyle associated with acl teararthroscopy techniques june 20.
This kind of disease is commonly seen in the knee joint sprain during strenuous activity. Because this mechanism is similar to. One observational study by duany et al.
Bone marrow edema is noted in the inferior pole of the patella consistent with contusion. If a patient does not have subchondral collapse and fails conservative treatment, they may undergo a core decompression and arthroscopy. With 15 patients reported an 87% success rate with joint preserving surgery that included core decompression, arthroscopy and autologous graft transfer [14].
No significant edema at the subchondral fracture likely chronic. Shaver used to debride unstable flaps of cartilage off the medial femoral condyle Pain resolution, significant improved function, and range of motion were the end results of our instituted treatment plan.
Description of procedure (abridged) medial compartment: To achieve this, bioabsorbable sutures are used to suture. Trochlea, medial femoral condyle, lateral tibial plateau;
Treatment of a femoral condyle fracture.
Generally, treatment for an avulsion fracture includes: Management and treatment how are avulsion fractures treated?
Medial collateral ligament avulsion femur Image
Posterior cruciate ligament avulsion fracture;
Avulsion fracture knee treatment. In this avulsion fracture treatment, a cast is placed on the fractured area for anywhere from four to six weeks. The knee joint remains particularly susceptible to avulsion fractures due to its numerous tendinous, ligamentous, and meniscal attachments. Anterior cruciate ligament avulsion fracture;
Injuries like this, if gone untreated, can lead to further damage and lifelong pain. However, conservative treatment often causes some complications, such as synarthrophysis, nonunion, joint instability, and arthritis, resulting in an unstable fixation and an unsatisfactory outcome. Treatment of an avulsion fracture typically includes resting and icing the affected area, followed by controlled exercises that help restore range of motion, improve muscle strength and promote bone healing.
How is avulsion fracture of the knee treated? How long does it take to recover from an. Arthroscopically loop or transosseous can be fixed.
However, if the fracture is. Clinical and radiographic findings confirmed the presence of an avulsion fracture at the proximal attachment of the mcl, combined with complete anterior cruciate ligament (acl) and posterior cruciate ligament (pcl) rupture. The treatment method was not standardized and was determined by the patient, their parents, and the treating physician regardless of the presence of avulsion fracture.
Origin of mcl avulsion fracture: Most avulsion fractures respond very well to physiotherapy treatment & only severe cases require surgical intervention. But in the condition of, even though very uncommon, tibial tubercle avulsion fracture, surgery gives a better outcome and resolution.
Doctors also recommend that this be paired with ice therapy, where ice is applied to the injured area for 20 to 30 minutes every three to four hours, or during times of swelling or pain. Most avulsion fractures are treated conservatively with pain and swelling control and early return to activities. Keep weight off the ankle until it has healed, and take measures.
Most avulsion fractures heal very well without surgical intervention. Treatment depends on which bone broke and the type of avulsion fracture. Displaced avulsion fractures require surgery.
Avulsion of the medial collateral ligament. To find out more, contact naas physio clinic on: Commonly, conservative treatment and surgery are the two major treatments of avulsion fracture.
An avulsion fracture occurs when a small chunk of bone attached to a. If the fracture is small, it can be treated with as little as rest, ice, and a bandage. Removing small portions of the kneecap that cannot be reconstructed may also have good results.
Avulsion fractures of the knee are numerous due to the many ligaments and tendons inserting around this joint. If the kneecap is broken in many pieces at its center and the pieces are separated, your doctor may use a combination of wires and screws to fix it. Immobilization in a cast or splint.
An avulsion fracture involves the detachment of a bone fragment that results from the pulling away of a ligament, tendon, or joint capsule from its point of attachment on a bone. Complete removal of the kneecap is a last resort in treating a comminuted fracture. Open reduction and internal fixation with a screw can be done.
The main treatments for an ankle avulsion fracture are rest and icing. Ofter bracing or splinting are used. Treatment of an avulsion fracture typically includes resting and icing the affected area, followed by controlled exercises that help restore range of motion, improve muscle strength and promote bone healing.
Even a small bone chip (avulsion fracture) should not be taken lightly. Most avulsion fractures heal very well without surgical intervention.
Courses, webinars, and online events, in your region or worldwide. The bone can fracture in different ways.

Hip Dislocations, Femoral Head Fractures, and Acetabular
The rod passes across the fracture to keep it in position.

Femoral head fracture treatment. Femoral head fractures are rare traumatic injuries that are usually associated with hip dislocations. It can sometimes happen after an acl reconstruction. A closed reduction should be attempted, in the interest of time.
When surgical intervention is indicated, there are multiple approaches that can be successfully and safely used for definitive fixation. The first phase of treatment is to reduce the femoral head, if dislocated. Further endeavor to improve the outcome should be taken.
Open reduction and internal fixation of the fracture of the femoral head is the treatment of choice for most young patients. The standard of care for a displaced fracture where the blood supply is disrupted involves replacing the femoral head (hemiarthroplasty or a total hip. Controversies include the preferred surgical approach (anterior versus posterior) and whether to perform femoral head fragment excision or internal fixation.
Metal screws are inserted into the bone to hold it together while the fracture heals. Wide treatment options for pipkin 1 femoral head fractures range from fragment excision, fixation following open reduction with internal fixation, or conservative treatment such as close reduction alone after fracture dislocation. Femoral head fractures are associated with posterior and anterior dislocations of the hip.
Treatment may be nonoperative or operative depending on the location of the fracture and degree of fracture displacement. An intramedullary nail can be inserted into the canal either at the hip or the knee. Open reduction and internal fixation (orif) of femoral head fracture is the preferred treatment for most patients.
Fracture management with minimal resources. Small series constitute the majority of the available literature. Femoral stress fractures take several months to fully heal.
Your upper femur and the socket in your pelvic bone are replaced with artificial parts (prostheses). Currently, the method most surgeons use for treating femoral shaft fractures is intramedullary nailing. Sometimes screws are attached to a metal plate that runs down the femur.
Femoral head fractures are associated with a posterior hip dislocation and acetabular fracture, although the fracture can occur in the absence of either of these conditions. The femoral head or the acetabulum significantly change the treatment. Revised distal humerus module is.
Surgical approach and fracture management is variable. Fracture healing can be attained in all femoral head fractures by using open reduction and screw fixation. In younger patients, preservation of the native femoral head allows full return to normal activity and low risk of future complications if the fracture heals ( 1 ).
In some selected cases when there is a very small fragment located in the region below the fovea, removal should be indicated. The treatment of a supracondylar femur fracture is highly variable and may involve a cast or brace, an external fixator, an intramedullary rod, or the use of plates and screws. Our results by using conventional approaches were associated with high complication rates.
23 hip dislocations require urgent reduction because the vascular supply to the femoral head may be compromised. Surgical dislocation approach has shown some promise in improving the. Most fractures of the femoral head are treated surgically, given the tendency for these fractures to have displacement and joint incongruity.
23 management of hip dislocation without fracture includes closed reduction under conscious. However, the optimal surgical approach for the treatment of femoral head fracture remains controversial. The fracture occurs on the femur close to the knee.
The use of the transtrochanteric or. Treatment consists of urgent closed reduction of the dislocated hip followed by nonsurgical or surgical management of any associated fractures. And outcome of a hip dislocation.
Hip dislocations associated with a fracture either of. How long does it take for a femoral stress fracture to heal? Associated fractures of the hip itself, such as acetabular wall fractures and femoral head fractures, may require surgical intervention even if the hip dislocation can be reduced in a closed fashion.
During this procedure, a specially designed metal rod is inserted into the canal of the femur. The primary goal of treatment for proximal femoral fractures is restoration of the patient’s normal functional mobility. Background femoral head fractures:femoral head fractures:
The treatment of femoral head fractures associated with acetabulum fractures, pipkin iv fractures, presents difficulty as usually the femoral head. The one exception to this is if there is a femoral neck fracture, at which point open reduction is almost certainly necessary. Stop any moderate activity and repetitive, stressful exercises (running, squatting, cycling).
Operative treatment of displaced femoral head fractures can be either in the form of internal fixation or simple excision of the fracture fragments. How femoral fractures are treated. Treatment a femur fracture is always considered a medical emergency requiring immediate evaluation and treatment in a hospital.
There are several surgical approaches and treatments for this difficult fracture.
The tibia is the shin bone. If the stress injury is significant, pain may persist at rest, too.

Shin Fracture or Fracture of TibiaCauses, Symptoms, Types
It is the new cells along the line of the fracture which will become visible.
Shin stress fracture treatment. 733.93 tibial stress fracture 719.46 lower extremity pain tibial stress injuries, commonly called “shin splints”, result when the bone remodeling process adapts inadequately to repetitive stress. Unlike shin splints, the treatment for stress fractures will vary based on the location and severity of the fracture. It can be difficult to distinguish a tibial stress fracture from a case of shin splints.
It merely refers to pain that occurs in the area of the shinbone (tibia bone). Home remedies for stress fracture. Pain is often localized in one spot, rather than a spread out over a small area, as with shin splints.
To protect your skin, wrap the ice packs in a thin towel. So making sure you're treating your shin splints appropriately and doing the right thing so they don't progress and get worse. Physiotherapy is an important treatment for a stress fracture of the tibia.
Constant impact force can lead to a stress fracture if the muscles are not strong enough to “absorb the shock.” seek the advice and treatment of a physical therapist if you experience shin pain. It’s important to give the bone time to heal. This article will cover a range of reasons why a person may have shin pain, as well as symptoms, treatments, and how to prevent them.
[6] in addition to the conservative methods, doctors typically recommend the use of an orthotic device, such as a walking boot or brace with crutches. People who have flat feet or recurrent problems with shin splints may benefit from orthotics. A shin splint and a stress fracture bear similarities in terms of medical management.
That beginning area is going to be sort of shin splints. [5] the tibia is the larger of the two bones in the lower leg. Treatment includes getting adequate rest and backing off intense exercise until it heals.
And that's when you get closer to that stress fracture. Thus, a tibial stress fracture is often called “shin splints”. This may take several months or even longer.
To ensure proper healing, i often place the runner in a walking boot and may even add crutches. Wearing shoes with good cushioning during daily activities will help reduce stress in your shins. A stress fracture of the lower leg in the area of the shin is generally considered an overuse injury.
High risk stress fractures in grade 1 or 2 categories (table 2) typically resolve nonsurgically with immobilization and weight bearing modification, and return to activity only after the fracture has achieved complete healing is essential to avoid full fracture.1,24 the selection of surgery as a treatment choice should be a decision between the athlete and sports medicine. You can treat shin splints at home by applying ice packs to the painful area for 15 to 20 minutes at a time, four to eight times a day for several days. A stress fracture of the tibia is an incomplete fracture or crack within this bone.
Apply ice packs to the affected shin for 15 to 20 minutes at a time, four to eight times a day for several days. Shin stress fractures can occur due to cumulative trauma to the bones, and the result is a small crack or fracture in the bones of the lower leg, often not visible on radiographs. A tibial stress fracture is not a specific injury.
Runners with a stress fracture have to stop running until it heals. Pain such as a stress fracture. However, stress fracture requires more limitations in movement to prevent injury progression.
Surgery also might be an option to facilitate healing for elite athletes who desire a more rapid return to sport or laborers whose work involves the stress fracture site. Two simple modifications with running that can also help with avoiding further shin splint aggravations are: Trigger point massage applied to gastrocnemius muscle by specilaist therapist.
Shoe inserts can help align and stabilize your foot and ankle, taking stress off of your lower leg. The mri is the best way to diagnose a stress fracture. Shin splints can usually be treated at home.the following suggestions may help to relieve the pain and allow your legs to heal:
Although unusual, surgery is sometimes necessary to ensure complete healing of some types of stress fractures, especially those that occur in areas with a poor blood supply. Controversy and confusion exists with the term shin splints. What is the best treatment for a stress fracture?
It usually takes 6 to 8 weeks for a stress fracture to heal. Recovery timelines can vary from 2 weeks to 4 months based on grade of injury, time to diagnosis, and patient compliance. Run for only one mile every other day for the first week and no more than two miles in the second week.
Stress fractures are point tender at the site of the fracture. Orthopaedic surgeon, and the staff at Treatment for mtss is contingent upon both severity of stress injury, relative risk, and stage of injury at diagnosis.
The first treatment is to calm the inflammation and control the swelling and pain. This can be managed with the r.i.c.e.p approach to treatment, as. After full recovery, simple running in gradual stages should be started.
According to the american academy of orthopaedic surgeons (aaos), shin splints are a common cause of shin pain, there are many other causes of shin pain, such as an injury, bone bruise, or stress fracture. Often you then see new. Continue with this system until you are running ten miles at the end of ten weeks.
So is a stress fracture basically the bone developing cracks in it because of repeated force? How can i treat my shin splints?
Initially, a spinal stress fracture is treated using conservative, nonsurgical methods. Patients will need to take a break from the activity that caused the stress fracture, as well as any other activities that put stress on the lower back.

Lower Back Stress Reaction/Stress Fracture Treatment
In previous posts, we have discussed chronic overuse injuries to the upper and lower limbs.the last area of discussion in regard to common youth injuries is stress injuries to the lumbar spine.
Lower back stress fracture treatment. Exercises to strengthen spine and surrounding muscles Surgery may be recommended for spondylolisthesis patients with severe slippages, or for those whose back pain has not improved with nonsurgical treatments. Postural exercises to encourage correct posture so you’re not overstressing your healing lower back
Treatment for stress fractures usually involves rest while the bone heals and changing your activity. A stress fracture is a very small crack in the bone. What is lumbar stress fracture?
Treatment aims to reduce pain, restore range of movement, develop core stability and functional strength. “treatment for these types of stress fractures is rest from extension activities, which often means a period of recovery ranging from a couple of weeks to several months depending on the. Physical therapy is important in maintaining range of motion and promoting strength and flexibility of the soft tissue.
Therefore, we utilise a combination of the following treatment methods: Implement strength training at an early age. Physiotherapy has been highlighted to be an effective treatment for lower back stress reaction / fracture.
Core strengthening is also very important as these are the deep muscles that help to support your lower back. To reduce swelling and relieve pain, your doctor might recommend applying ice packs to the injured area as needed — 15 minutes every three hours. There may also be multiple fractures that you are unaware of.
Exercise with a swiss ball to increase lower back muscular stability; “the examination usually reveals tenderness over the lumbar spine in the lower back and pain with extension, particularly when leaning back standing on one leg versus the other. Stress injuries can be found in the shin bone, foot, heel, hip and lower back.
The treatment for a stress fracture of the back is conservative, with pain medications and rest, to allow the bones to heal in almost all. Consult a sports injury expert; It is a common cause of structural back pain in children, adolescents and active young adults.
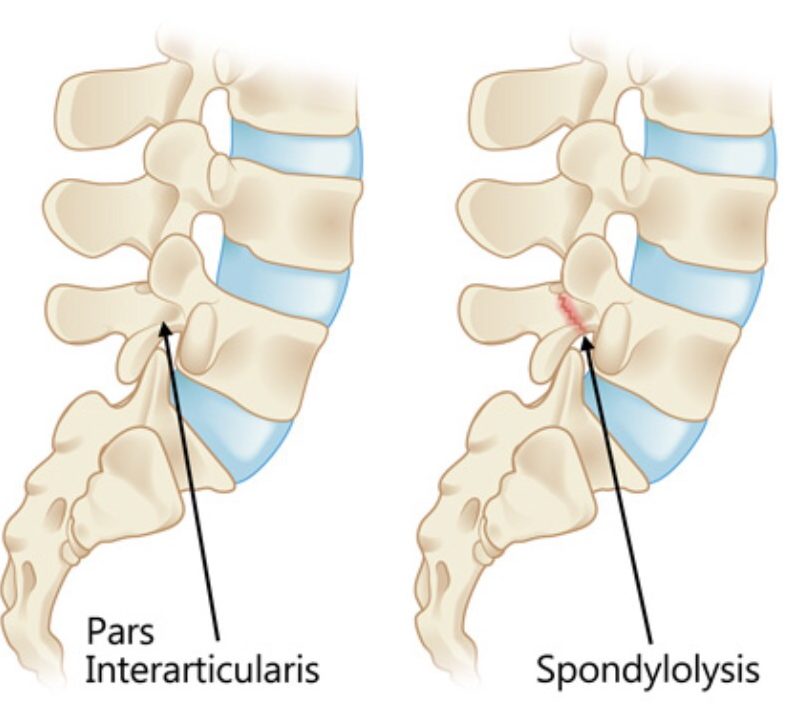
Obviously, i want to avoid painful motions like lumbar hyperextension and rotation. Its the fracture of the lumbar spine at the level of the lower back above the sacral spine its caused by sitting or falling down on your back. Repeated microtrauma to the pars interarticularis is usually to blame.
Stress fractures also occur in other nearby areas due to the same mechanism of repetitive loading without adequate recovery. Treatment involves a complete rest from sporting activities, for a period of six weeks to allow the bone healing. How can you avoid a stress fracture?
Can a fractured vertebra in. Other treatments for severe injury to the lower spine are electrical stimulation of the injured bone area and surgery involving lumbar. A spondylolysis in a child or adolescent most commonly results from a defect or.
If you injure your lower back, lie down and take the weight off you back, place a cold ice pack over a washcloth to prevent frostbite, and decrease swelling and reduce your pain, by numbing the affected area, until you can get medical treatment. However, back braces are most effective when the fractures are the lower back (lumbar spine) or in the lower portion of the midback (thoracic spine). Wear a back brace to provide immobilisation & support;
Just like any bone fracture, stress fractures in the low back need time to heal. Brace used to help restrict motion during a low back stress fracture these are just some of my quick and easy exercises to help promote movement in the spine. A soothing heat pack can reduce back pain and alleviate back muscle spasm in the early stages.
The predominance of stress fractures in the lower limbs, over fractures in the upper limbs, reflects the cyclical overloading that is typically exerted on bones that bear the body weight, in comparison with bones that do not have this function.3 stress fractures are mostly commonly diagnosed in the tibia, followed by the metatarsals (especially. Back braces can provide some stability to the spine and thereby reduce pain. Use a seat support to improve posture whilst sitting;
In most cases, symptoms will go away after a period of rest. More serious stress fractures may take a little bit longer time to heal and get back to normal activity. Initial period of rest to offload structures which varies for severity and.
The most common treatments for lumbar stress fractures are sufficient rest periods and physical therapy which will commonly include “core strengthening” exercises. Cricket fast bowling is a unique asymmetrical action that loads the trunk through rotation, extension and side flexion at the delivery stride. In the meantime, patients can take.
What should you do if you suffer from a lower back stress fracture? A stress fracture can occur in adolescents who participate in sports that involve repeated stress on the lower back, such as gymnastics, football, and weightlifting. Treatment of spinal stress fractures.
This means resting from all sporting and impact activities until there is little, to no pain. In majority of the cases, with treatment, it takes about 12 weeks for an individual to completely heal from a stress fracture of the back. The image below shows the most common area for stress fractures known as the “pars interarticularis”.
The main treatments are wearing a back brace for three to six months to support the lower lumbar area, limiting the activity that caused the injury, and doing physical therapy exercises. The pars is particularly susceptible to injury in young people, particularly in athletes. Measures should be taken to ensure that nutritional values are met by making adjustments to the athlete's diet.
A stress fracture in your spine is known as spondylolysis. This action repeated time after time can lead to the development of stress fractures in adult and adolescent populations. Low levels of calcium and vitamin d affect bone density and may increase the risk of a stress fracture.
A physical therapist, personal trainer, or rehab specialist may recommend a pain management and recovery plan for a lower back stress fracture that includes: In patients with a bilateral stress fracture, there is a rare complication where spinal alignment could be affected. The main injury of focus is spondylolysis, more commonly known as a stress fracture or stress reaction, and is defined as “a weakness or stress fracture in the bony arch of.
Yes, it would hurt and eventually your lower back will lay the price. In some cases, the stress fracture weakens the bone so much that it is unable to maintain its proper position in the spine — and the vertebra starts to shift or slip out of place. Maintain fitness in the pool with a buoyancy aid;
The medical term given to lower back stress fractures is a “pars fracture” or “spondylolysis”. With a lower back sprain and fracture you want to off load the. You can be icing your back once an hour for 15 minutes.